The demand for automated enrollment solutions is growing rapidly. Processing enrollment data quickly and accurately is critical for members to access the care they need, when they need it. Health plans today need an experienced partner that provides a scalable data management solution, backed by powerful data insights and processing transparency.
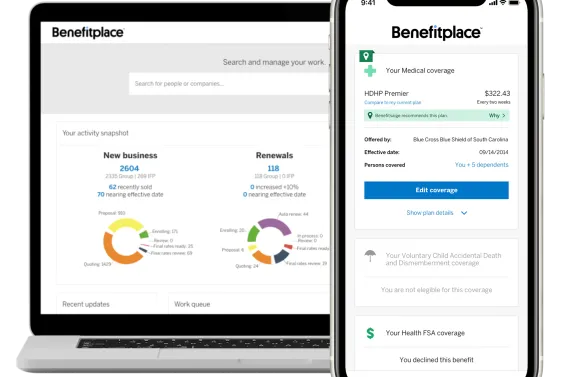
Data Management, through Benefitfocus, is a comprehensive solution designed for health plans to quickly and accurately process third-party data in a standard format, making enrollment seamless and more efficient. With more than 20 years of experience, our proven technology and white glove service offers health plans a total solution that can support individuals and groups of all sizes and a wide range of data formats and submitters - from benefit administration platforms to brokers - even during peak enrollment seasons.
And with our modern Data Management Dashboard, it’s never been easier for health plans and their customers to manage enrollments. At-a-glance, users can view enrollment statuses and easily identify which were successfully processed and which may need attention. Insights and trends help quickly identify “hot spots,” such as submitters with a higher volume of processing errors where consultation may be needed to improve data quality and timeliness.
There’s also a member-level view, ensuring any discrepancies are identified and resolved quickly, before they impact coverage. Finally, we’re making it easy to take action right from the Dashboard, like re-processing transactions with errors after they’ve been reviewed and resolved.
Contact us to learn more about how Data Management through Benefitfocus can help streamline your enrollment experience today!